Chronic Disease Management: Tech's Role in Fighting Diabetes
/As a vehement supporter of value-based care models in care delivery, I am constantly amazed by the innovative ways these providers seek to control their medical costs. Telehealth, transportation, and even temporary housing have all been in the news recently for their promises to provide greater access while controlling exacerbations that lead to expensive ER visits. While I avidly support this type of innovation, I am a skeptical if any of these solutions will have an outsized impact - particularly within high risk populations. Instead, value-based care models are often successful because they do many of the little things right rather than just one big thing. As such, I wanted to explore some of the foundations of population health strategies, and I decided to begin my research with one of the most prolific chronic diseases facing our society: Diabetes.
What is Diabetes?
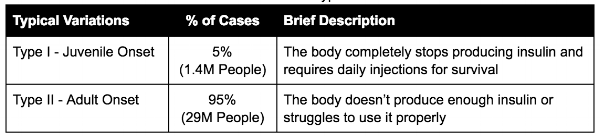
I was appalled by how little I knew about the disease before beginning this research. For those in a similar boat, here is a quick definition: Diabetes is a disease in which the body is unable to properly use and store glucose (a form of sugar). Glucose backs up in the bloodstream — causing one’s blood glucose (sometimes referred to as blood sugar) to rise too high. (Joslin Diabetes Center). Insulin, the common treatment for some types of diabetes, is a chemical typically produced by our bodies to control these glucose levels. This definition can be further broken down into the types outlined below:
Additionally, up to 9% of pregnant women get gestational diabetes (American Diabetes Association) and only 11% of the 84M people with prediabetes (high glucose levels below diabetic thresholds) realize they have it.
What are the impacts of this disease?
Individuals with diabetes can live relatively normal lives with proper management of the disease. However, when not closely monitored, the results can be deadly. Heart attack, stroke, blindness, kidney failure, blood vessel damage, and nerve damage all sound like the rare side effects we hear about on drug commercials - but these are common outcomes for diabetic patients that do not adhere to a proper management regimen.
At the very least, diabetics often spend the rest of their lives hyper-focused on the foods they eat, the timing of insulin injections, and consistent follow-up with a multitude of physicians. This is an incredibly difficult task for otherwise healthy individuals, let alone for parents with diabetic children and people with several other health and social challenges. Because of the difficulty of proper management, diabetics constitute a significant proportion of costs to the healthcare system: $237B of direct costs and $90B in productivity costs in 2017 (American Diabetes Association). Treating each individual with diabetes costs on average $16,752 per year - about 2.3x more than the average citizen. These costs are distributed across the ecosystem, primarily stemming from inpatient admissions - broken down as follows: hospital inpatient (30%), prescription medicine for complications (30%), anti-diabetic agents and supplies (15%), physician offices visits (13%), Other (12%).
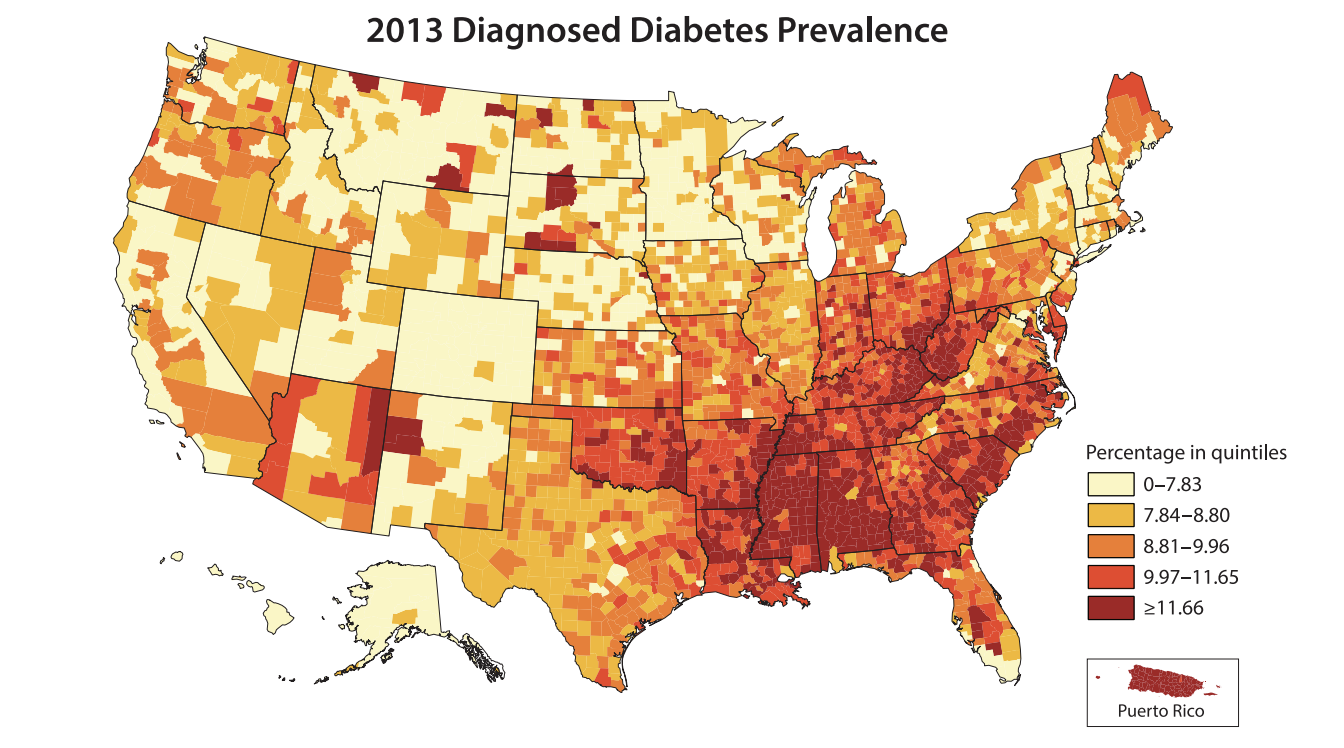
With 66% of the diabetic population on public healthcare programs (Medicare, Medicaid, etc.), the American taxpayer is footing most of the bill for these costs. However, it is the 2% of diabetics who are uninsured that constitute the greatest relative costs as they experience 68% more ER visits than insured patients.
To put that in perspective, diabetes costs the US more than the GDP of 29 countries across the world (Wikipedia)!
What causes diabetes and how is it treated?
Shockingly, we know very little about what causes diabetes despite the billions of dollars that have been poured into research over the past decades - this is a very hard problem. However, we have been able to identify several of the risk factors that contribute to the likelihood of contracting it, namely: family history, high cholesterol, high blood pressure, physical inactivity, and obesity. (Note: Beyond family history, the other factors above and below are typically associated with Type II diabetes risk and treatment).
Once you have been diagnosed, glucose levels must be consistently monitored (up to 10 finger sticks a day!) and insulin delivered via a needle or a pump as required. For Type II sufferers, not all patients need insulin to manage their disease, but many still do. Combine this monitoring with active meal planning and regular appointments with primary care physicians, dietitians, exercise physiologists, ophthalmologists, behavioral psychologists, and podiatrists, and it becomes easy to imagine the immense physical, mental, and emotional strain that managing the disease can present.
The pain and stress associated with management is why early risk detection and behavior modification prior to diagnosis is highly preferred to active treatment. Many of the risk factors mentioned above can be addressed with proper diet and exercise. As millions of new years resolution-ers find out each January, it is easier said than done. This is also compounded by the fact that a large portion of diabetics have several comorbidities and hail from lower socioeconomic segments of society. Choosing the right foods and finding time to exercise become significantly more difficult when you are food insecure, housing insecure, and/or support a family on a minimum wage salary, among other things. It certainly makes getting up to hit Equinox for an early morning Zumba class followed by a kale smoothie sound like a cakewalk (maybe cakewalk is the wrong term here - but you get it).
The Role of Technology in Diabetes Management
In helping combat diabetes, technology plays two key roles: monitoring and delivery and behavior modification. Let’s start with the former.
Monitoring and Delivery
Insulin was first discovered and injected in 1922 at the University of Toronto. Since that time, many medical device companies have been gradually inventing new technologies to make the measurement of glucose and delivery of insulin easier, safer, and more effective. Today, glucose monitors and test strips can be found and purchased at most major drug stores at relatively inexpensive prices - greatly improving access to the tools needed by millions across the country.
After measuring glucose levels, many diabetics still rely on syringes or pens as the tried and true method for delivering an accurate dose of insulin for their condition. However, there has also been extensive innovation through the development of pumps that provide a steady, highly accurate insulin infusion at the push of a button. These devices tend to be more expensive (around $5,000) and also require the user to wear them on their body at all times.
While the above devices have saved and extended countless lives throughout the 20th century, recent years have seen the development of new technologies that have revolutionized the process of monitoring and delivery. “Artificial Pancreas Technology”, as it is often called, provides continuous glucose monitoring (through either an implanted device or a patch), and delivers insulin via a hybrid closed loop system that automatically infuses a dose when needed. The user only needs to interact with the system when changing patches or calibrating the devices. It is nothing short of astounding and greatly improves the lives of Type I sufferers. Great examples of these devices can be found here:
Note: There has been a lot of news lately about the skyrocketing cost of insulin that I consider out of scope for this post. With that said, making this drug more accessible should be of utmost priority to individuals looking to reduce the costs associated with improper management of this disease. However, one note of caution, we should not be comparing the prices of insulin from decades ago to the insulin available today. In many ways, it is a completely new product and we should consider this when determining a fair price for this vital compound.
Behavior Modification
The holy grail of value-based care is the ability to encourage healthier behaviors among plan participants. There really is no silver bullet as every individual has different motivations and reasoning for their actions that no customer segmentation could ever accurately represent. Technology is constantly advancing in the personalization of messaging and incentives to encourage meaningful lifestyle change, but tech alone will never be enough. With that said, there are several organizations that have developed services explicitly for diabetics that utilize technology to enhance their offerings. Here are a couple examples:
Omada Health - Omada has been, arguably, one of the most effective organizations at tackling the diabetes epidemic. By combining a wireless scale, a mobile-enabled application for tracking food intake and exercise, personalized coaching, and a support community, the organization has been so effective that they have developed an outcomes-based pricing model that only rewards the company when results are achieved. With ten peer reviewed studies completed at the time of this post, Omada Health has demonstrated an ability to greatly reduce the risk of being diagnosed with Type II diabetes within specific populations (by 30% according to their website). This is the power of tech-enabled services.
Virta Health - Virta has taken a nutrition focused approach to tackling diabetes, while also combining physician services with IoT devices like a wifi scale. The primary focus of the model is getting patients onto a ketogenic diet and providing them with the physician support needed to manage their disease. The organization claims to reverse diabetes in 60% of their patients that meet certain criteria. Amazing!
Conclusion
Given the prevalence of diabetes across the US and the relatively high proportion of medical costs that it drives, developing new models to address this epidemic remains a high priority in the value-based community. Technology can certainly help with management and behavior modification, but it must be combined with a suite of services to have the greatest impact. I hold out hope that medical science will eventually develop a cure for this disease, but - in the meantime - it is clear we are making significant progress in improving the lives of the millions of people diabetes affects every day. When that day comes, we will be faced with another huge challenge - the lost $200B a year medical device, pharmaceutical companies, and providers generate from treating the epidemic. They will almost certainly do all they can to delay the introduction of such a treatment to the market if the “fee for service” system persists. In the words of Elisabeth Rosenthal, a Harvard-educated physician and writer for the NYTimes, “a lifetime of treatment is preferable to a cure” [in the US healthcare business].